Our health series shines a light on Obsessive Compulsive Disorder in the May|June issue, out now
In the new issue of Irish Country Magazine, our award-nominated health series The Invisible Struggle spotlights OCD, and breaks down its harmful stereotypes and stigmas, as well as sharing expert advice in how to treat this debilitating condition. In the feature, Niamh Devereux speaks with three Irish women who live with OCD, who share their stories. These were condensed for the magazine: here are their accounts in full here – trigger warning, they may be upsetting for some to read. Here, we spotlight more voices who wish to spread awareness about OCD and share what it’s like to live with.
What are your earliest memories of experiencing symptoms of OCD?:
Anonymous: I think my intrusive thoughts began when I was under ten years of age but certainly I know at 15/16 years old these were present and had started to cause distress to me.
Grainne Maloney, 27, Co Kildare: My earliest memory of what I know now to be OCD was when I was a child. If a thought came into my mind I would immediately tell my mother the thought, which would make me feel better, and I would turn the handle on the bathroom sink a number of times in order to feel relief or comfort. It developed in my teenage years into writing constant lists of things that popped into my head, things such as books, songs, movies or just words. I wrote these lists in my school homework journal so I could look back on them when I got home.
Brian Clarke, 32, Co Meath: My earliest memories of OCD stem from childhood, as far back as the ages of six/seven I can remember having OCD tendencies. I always had a deep feeling of being different in some way. I tended to think a lot more deeply. I had irrational thoughts and beliefs. I have been having intrusive thoughts since I can remember.
Many people have unhelpful stereotypes in mind when they think of OCD. How does your OCD present itself?:
Anonymous: My OCD is typically referred to as ‘Pure O’ by sufferers. My intrusive thoughts, the thoughts that accompany any and all OCD themes, are rooted in childhood trauma. OCD is so much more the compulsions such as cleaning or turning light switches on and off. My OCD is deeply upsetting to me and has taken years of life from me in terms of being able to be in a workplace and being able to interact with friends and other people.
Grainne: Now I am in my late twenties and my OCD presents itself a bit differently. I experience intrusive thoughts, as well as false memories and with that comes a lot of anxiety. I’d like to mention I’m also autistic. I mention this as there’s many people with autism and OCD, and they can have many similarities.
Brian: Most people with OCD have intrusive thoughts or have had at some point. They can vary in themes; mine centred around harm OCD. I believed if I had a bad thought it meant I was responsible or that I wanted it to happen. I felt responsible for the safety of others, I can remember praying or having mantras that I would say to myself over and over to “rid” the bad thought. I became a compulsive hand washer, I was terrified of germs, I would wash my hands to the point they were cracked and bleeding. In later years my OCD developed into mainly intrusive thoughts.
What would you really like people to know about this condition and what it’s like to live with?:
Anonymous: This condition can be absolute living hell especially when the average time for a person to be diagnosed with OCD, according to what I’ve read, is approximately ten years. I wasn’t diagnosed until well after this ten year period, and so medication and appropriate CBT therapy took ages to get. People with OCD are not bad people, they are living with a condition that takes over their ability to function.
Grainne: I’d like people to know it’s not just a condition where you wash your hands a hundred times a day, Sure, that can be a part of a broad spectrum that is OCD. I have heard many people say “I am so OCD” because they like to organise things – unless that is giving you anxiety and really interfering with your daily life, it’s not OCD, you just like to be organised. As someone who suffers with this condition it’s difficult to hear that, as it belittles the experience many of us go through. In addition there are many types of OCD that are not as well known, like contamination OCD, such as Relationship Obsessive-Compulsive Disorder, Harm OCD and Pure O. I’d like people to know how exhausting and stressful it is to live with daily. I really commend every person living with this condition because it takes a lot of strength to keep soldiering on with what feels like the weight of the world on your shoulders.
Brian: Sadly there are many unhelpful stereotypes around OCD and I have witnessed them all. It can be very infuriating. The biggest stereotype I find is the idea that people with OCD are “clean freaks” or that we somehow like to have everything in order or symmetrical. Whilst it’s true in some cases it’s not for all of us, having things clean and organized is usually a compulsive response to intrusive thoughts. It doesn’t mean to say the person enjoys it. Lots of people have clean homes or desks, it does not mean they have a mental health condition. So why would you say that of people with OCD? There are a lot of things I’d like people to understand about having OCD. The main one is that OCD is not a quirk, and it’s most definitely not one bit enjoyable. It can be horrendous to live with, for 20 years I’ve been having intrusive thoughts, they have changed themes over the years but have always been disturbing. When you tell someone you have OCD, they always say “oh everyone has that” or “I am a bit OCD myself” or the classic “you must have a tidy home”. When you explain the nature of the thoughts and compulsive behaviours, they soon take a different view and it’s suddenly not very appealing. It is a terrifying disorder.
Are there any particularly challenging moments you can recall?:
Anonymous: When I was in my absolute worst peak of OCD intrusive thoughts, getting to sleep and just functioning without getting an anxiety attack well over 15 times a day was the hardest part of my recovery. Self-harming was unfortunately something I turned to during this time but in the long run it doesn’t solve anything. Getting professional help is what kept me going during the challenging times.
Grainne: There isn’t just one moment that I’ve found extremely challenging to deal with when it comes to OCD, but many. Because of my OCD, I’ve avoided people, places and things in fear of getting an intrusive thought. I have also experienced severe panic which can be debilitating. Additionally I have suffered false memories which is where the brain tells you something has happened but it didn’t. For example, one could have a false memory concerning a car crash or cheating on a partner. Seeing other people experience life without excruciating fear and doubt can be really hard and discouraging for me and others living with OCD.
Brian: OCD has always been a challenge for me, throughout the last 20/25 years. I still have OCD today but I manage it with a combination of medication, therapy and on my own, I was first diagnosed in 2014. It was only after I became severely depressed over the course of a few years, I was living with horrendous intrusive thoughts that scared me, I thought I was completely mad, and that I was going to be locked away forever, I thought I was a danger to people. I had at this point become suicidal, and was very close to taking my own life on a number of very dark occasions, until I told people what was wrong.
Have you received a diagnosis, and how was that process if so?:
Anonymous: Yes, I have Mixed Anxiety Disorder with OCD attached. This process of diagnosis was something I had to push for and I had to find a professional because I was never referred to a professional. Treatment using professional CBT therapy is what got me through along with the proper medication that worked for me.
Grainne: I first got help by going to a psychotherapist and eventually started to go to support groups. One difficulty of anybody experiencing OCD in Ireland can be the difficulty of getting a diagnosis, if you go publicly to see a psychiatrist you could be on the waiting list for years, and if you go privately it can be extremely expensive for each session. I have been on the public waiting list for over a year because I don’t have hundreds of euro to spend on a private psychiatrist.
Brian: Eventually, after a number of hospital visits, and being put on all sorts of medication, I eventually got diagnosed with OCD in July 2014. Today I manage my OCD with medication which works for me. I have attended a psychiatrist for a few years, I underwent cognitive behavioural therapy for six months which is the main treatment of OCD. The idea of CBT is about accepting thoughts and not interacting with them or giving them power. It’s an incredibly simple technique but very powerful. I also practice meditation daily, I walk almost every day, I read a lot of books on spirituality, the
mind and religion. All of this combined helps to keep the mind active, and in turn keeps OCD at bay. I also set up a support group in Meath for those with OCD. There is not enough support out there for people with OCD.
For those living with OCD, or who suspect they may have OCD, what is your advice for them?:
Anonymous: Get both a doctor’s opinion and a second opinion from a specialist. Opening up to the wrong person who doesn’t professionally understand this condition can be detrimental to your own feelings toward your OCD. To anyone who is struggling with intrusive thoughts and OCD please know it gets better and life gets easier. Go to professionals and push for a diagnosis or referral or assessment. Don’t isolate yourself and keep contact with others either friends or people suffering from the same condition. Join a support group and go each week. Schedule a doctor’s appointment and go and ask them for help.
Grainne: As someone living with this condition the best way you can treat it is taking it day by day but by also taking part in different therapeutic techniques such as Exposure Therapy and Cognitive Behavioural Therapy. I think attending support groups, either in person or online, are extremely beneficial and important so you know you’re not alone in this condition. I also listen to The OCD Stories podcast which is amazing for information and to listen to others stories. There are many books about OCD which are also helpful; The Man Who Couldn’t Stop is one of my personal favourites. Working out helps me a lot because I get some time to focus on exercise rather than what’s going on in my head. It’s also important to remember that some days will be better than others and vice versa. If you have OCD or suspect you have OCD, get help for it. It can be a very isolating experience but there are so many people out there that are going through the same struggle. As well as seeking support, be kind to yourself and take credit for continuing the dark journey of OCD.
Brian: My advice to anyone who thinks they have OCD or that they have it, is to get help as soon as possible. It will never get better unless you get treatment, thankfully today there is far more help, therapy and treatment out there for mental health conditions. Living with OCD and managing it daily is doable, and most live perfectly normal lives, and there is a lot of support and information out there to help you.
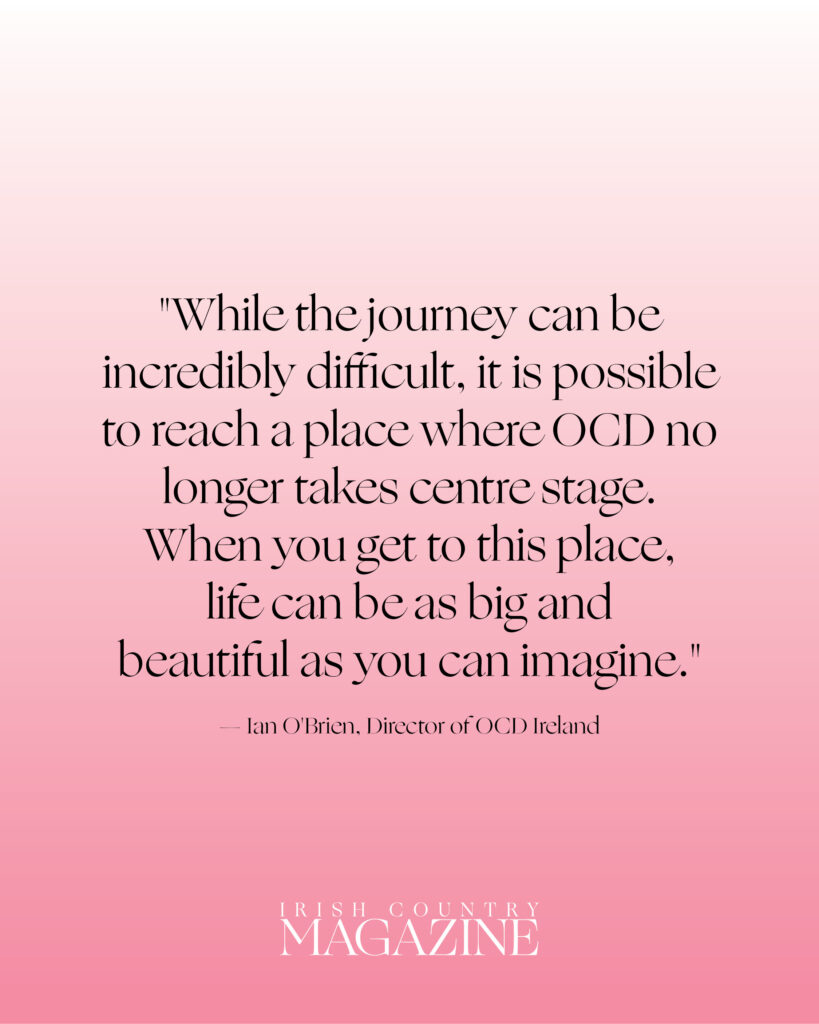
For more information – from Ian O’Brien of OCD Ireland and Professor Jim Lucey, an Irish psychiatrist with a special interest in obsessive compulsive disorders – and to read more stories, pick up the latest editor of Irish Country Magazine.
Obsessive Compulsive Disorder: need to know
- Obsessive Compulsive Disorder (OCD) is a mental health condition, characterised by recurring, intrusive thoughts – or obsessions – that trigger intense anxiety, leading to repetitive behaviours or rituals (compulsions).
- These are performed to alleviate discomfort and fear, and are driven by the belief they will prevent harm, even if there is no logical connection.
- In can present in different forms, or subtypes, including obsessions without visible compulsions.
- OCD affects thousands of people across Ireland, and yet many still only associate it with the stereotypes they’ve been fed through pop culture, where it’s reduced to a quirk, or a punchline.
- Obsessions are as varied as one can imagine; people can have intrusive thoughts (or images and urges) related to sex, violence, blasphemy, and so much more.
- Cognitive Behavioural Therapy (CBT), particularly Exposure and Response Prevention (ERP), is the gold standard for managing OCD, while medications like SSRIs can also be considered effective and helpful for those with moderate to severe symptoms.
- While some people respond well to ERP alone, others may achieve the best outcomes with a combination of therapy and medication.
- The first step is making a GP appointment. For further support, ocdireland.org provides free support groups, both online and in-person for people living with the condition and their loved ones, too.